40-year-old female presented with abdominal pain in the bilateral lower quadrants with radiation to the back. She had some nausea and vomiting but no hemetemesis or melena. With the pain, she had fatigue, weight loss (2 notches on the belt over 6 months). No other symptoms including pulmonary.
In 2002, the patient underwent an evaluation for bilateral pneumothoraces. Chest tubes were placed, and she had a prolonged hospital course. Her course was complicated by the discovery of a congenital hole in her right hemidiaphragm.and herniation/strangulation of a portion of her stomach into this area. She underwent closing of her diaphragmatic lesion and partial gastrectomy.
In 2005, she presented to an outside institution with a right-sided pleural effusion. She had a thoracentesis, but an etiology was never determined. She did not followup. She reports her last chest x-ray was performed in May of 2005. She is unclear as to what this showed.
PAST MEDICAL HISTORY: Uterine fibroids. PAST SURGICAL HISTORY: 1. Surgical repair of right-sided hiatal hernia.
2. Left herniorrhaphy.
3. Cholecystectomy
4. Appendectomy.
5. Congenital hearing abnormality. ALLERGIES: No known drug allergies.
SOCIAL HISTORY: The patient denies tobacco, alcohol or drug use. She is an aide for a Special Education Class in the Public School System MEDICATIONS ON ADMISSION: None. FAMILY HISTORY: Noncontributory
Exam: VSS, afebrile: Lungs: Decreased breath sounds on the right side from the base to the apex of her right lung. Her left lung was clear to auscultation without wheezes, crackles or rhonchi. There was right-sided decreased percussive resonance and decreased tactile fremitus. Abdomen: Soft, tender in the left lower quadrant without rebound or guarding. No masses appreciated. She has normoactive bowel sounds.
LABORATORY STUDIES ON ADMISSION: Sodium 136, potassium 5.2, chloride 101, bicarbonate 24, BUN 11, creatinine 0.7, calcium 10.5, glucose 129, total protein 7.7, albumin 4.5, alkaline phosphatase 74, AST 30, ALT 10, total bilirubin 1.1, direct bilirubin 0.5, lipase 20, white blood cell count 12.8, hemoglobin 12.5, hematocrit 38.6, platelet count 500, beta-hCG less than 2
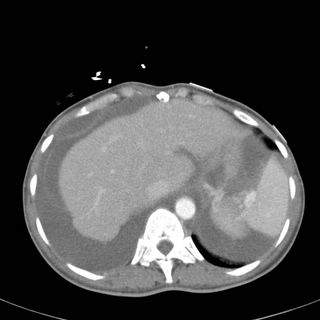
CT Images (obtained as the EC physician wanted to ensure the patient did not have a PE):


What do you do next? What is your differential diagnosis?
Update: See here for followup to this case (but read the comments below first!)
3 comments - CLICK HERE to read & add your own!:
It sounds like Meig's syndrome. The holes in diaphragm that you pointed out was likely your clue that the effusion was coming from the ascites. Thus, I would do an abdominal-pelvic CT to look at the ovaries and also get a CA-125 level.
The other effusion specific to woman is catamenial (Sp?)effusion from endometriosis but I'm not sure if she is post menopausal since I think that's mostly in child-bearing age.
The latter would give an exudative and the formaer a transudative.
I'll forgo on further DDx for effusion in general as the above 2 seem to fit with the story.
My thoughts are similar to jeff's. My gut impression while reading hte case was ovarian carcinoma. Of course, it's entirely possible that she does have an empyema that was seeded at the time of her chest tube placement for the pneumothorax. The mediastinum is shifted away from the effusion, suggesting that the effusion is "pushing" (as opposed to compensating for volume loss due to atalectasis or trapped lung).
Is there ascites and fluid around the liver in other cuts? In the last view, it looks like there is ascites, with fluid around the spleen and liver. Hepato-hydrothorax is a possibility, as is urinothorax, although neither really fits the clinical setting.
I would definitely explore the abdomen and look for ovarian carcinoma (in addition to tapping the pleural effusion and the ascites for standard studies. I'd include a triglyceride level with the pleural fluid analysis to r/o a chylothorax as can occur with LAM, lymphoma, or lymphatic obstruction by tumor).
There has been a great DDx listed so far. To be a purist, Meigs' syndrome is associated with benign ovarian tumor (though I think the term has been corrupted to include any ovarian tumor with this features).
I was obsessing a bit about the hearing disorder. I could not think of a clear syndrome with all this features. Congenital deafness is so multi-genic that it can be associated with almos anything. A classic systemic association would be with renal dysfunction (Alport's, Epstein's, etc.) but BUN/Creat were normal and didn't see a met acidosis.
The hearing disorder is probably more a red herring in relation to the new acute process. The diaphragmatic hernia was probably another small congenital abnormality that didn't quite build up to a syndrome.
LFT's were normal so a hydroTx from liver involvement would be less likely.
I guess we need a CT abdomen and data on the fluid itself as JJ suggested.
Post a Commenttest post a comment